Lay-Language Papers
Hybrid MRI-Radiation Therapy Machine for Improving Cancer Treatment
B. Fallone (ginofall@cancerboard.ab.ca), M. Carlone, B. Murray, S. Rathee, T. Stanescu, S. Steciw, K. Wachowicz, C. Kirkby
Alberta Cancer Board
Alberta, Canada
Author Summary of Paper TU-C-M100F-1
Tuesday, July 24, 2007
49th Annual AAPM Meeting, Minneapolis, MN
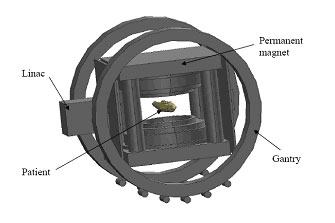
Currently being built in prototype form, this hybrid MRI-radiation therapy machine provides numerous advantages, including an unobstructed treatment beam, high-quality real-time imaging during treatment irradiation. (Courtesy B. Fallone et al., Alberta Cancer Board).
Radiation therapy is a proven strategy in the treatment of cancer. Despite all the modern technology used today in medicine, it is still difficult to see exactly where the radiation beam is located within the patient during radiation treatment. Because of this, the radiation treatment is not as effective as it could be since a conservative strategy must be used to ensure the whole tumor is treated and side-effects are as low as possible. By combining a radiation treatment machine with a magnetic resonance imaging (MRI) machine, it will be possible to precisely position the radiation beam on the patient’s tumor while the treatment is being given. In this manner, the full curing potential of radiation can be achieved resulting in improved treatment for cancer.
Modern radiation therapy relies on images (e.g., radiographic, computed tomography) as a guide to the placement of the radiation beam on the patient, using a technique commonly called Adaptive RadioTherapy (ART). However, modern techniques will always be undermined by two major problems. The present image guidance systems rely on 2D x-ray or 3D computed tomography (CT) x-ray images. These are good at seeing bones but poor for imaging organs or tumors. Also, x-rays and CT do not provide 3D images at the same time as the treatment. There are some workaround techniques, but these are invasive and problematic. Because of these problems, clinicians must apply larger than necessary treatment margins to ensure that the entire tumor is treated. This results in more side-effects, which can sometimes be serious.
In order to overcome the motion and poor tumor definition problems we are developing a radiation therapy-MRI system, which uses a process we call Advanced Real-Time Adaptive Radiotherapy (ART).2™ Combining a linear accelerator used for radiation treatments and an MRI is a difficult task because they function on scientific and engineering principles that make them incompatible with each other. The principal innovation behind our process overcomes these science and engineering problems. The linear accelerator and an open-bore MRI system are fixed with respect to each other, and rotate in unison around the patient, delivering treatments over all angles. This fixed-system concept will reduce interference between the linear accelerator and the MRI, and is protected under US and International patents assigned to the Alberta Cancer Board. The inventors are B. Gino Fallone, Marco Carlone and Brad Murray.1,2 The coupling of an MRI with a linear accelerator would allow the significant reduction of treatment margins during radiotherapy, which would result in better cures with less side effects.
Radiation treatments require complicated preparation and planning. Each patient receives a unique plan specifically designed for him/her. The preparation involves a complete set of imaging exams (e.g., radiographs, CT, ultrasound, MRI, PET) that are used in a complicated calculation process to organize the radiation beams for radiation treatment. Unfortunately, the position and sometimes the shape of the patient (and the internal organs) changes at treatment time. Currently appropriate technology does not exist to account for organ movements during treatment (for example lungs). Our system is being developed/designed specifically to account for patient changes and movements during radiation treatment. This is done by using stunning imaging provided by MRI at the time of the radiation treatment. This will represent a significant innovation in the manner in which radiation treatments are given.
At present, radiation treatments are used for cancers located in the head and neck, breast, prostate, rectum and elsewhere. However, its effectiveness is limited for cancers that exhibit motion, for instance due to breathing, because the radiation beam may not always be aimed at the tumor. The proposed system will solve this problem by tracking the moving tumor in real time with MR imaging, and adjusting the radiation beam accordingly. Our system will be beneficial for all solid cancers, but will especially benefit those cancers that are difficult to treat with today’s radiation technology, such as liver, stomach, pancreas, and significantly improve on others cancers where it is still difficult to administer sufficient radiation dose to obtain a good chance of cure, such as lung cancer, for example.
_______________
1B.G. Fallone, M. Carlone and B. Murray, Integrated External Beam Radiotherapy and MRI System 5625-35, PCT International Patent WO/2007/045076
2B.G. Fallone, M. Carlone and B. Murray, Real-time Dose Reconstructed Using Dynamic Simulation and Image-Guided Adaptive Radiotherapy 5625-34, PCT International Patent WO/2007/045075.