Emerging Role For HIFU Comes Into Focus
Emerging Role For HIFU Comes Into Focus
Highlights From Today’s Cutting Edge Medical Physics Research
In the 23 years since high-intensity focused ultrasound (HIFU) was first wed to MRI1 as a way to guide the placement of focused high-intensity ultrasound beams and provide real-time feedback on thermal targeting, the technology has shown increasing potential for surgery, oncology, and neurology at-large. With the many avenues at our disposal, HIFU offers the potential to dominate much of the therapeutic physics landscape in the coming decades, particularly as a reliable alternative to ionizing radiation therapy and minimally invasive surgery. Specifically, MRI-guided HIFU (MRgHIFU) has seen early success2 locating and destroying a variety of diseases, including cancer, through thermal ablation or locally delivering drugs and biologics. MRgHIFU is also a field rich with research opportunities in medical physics.
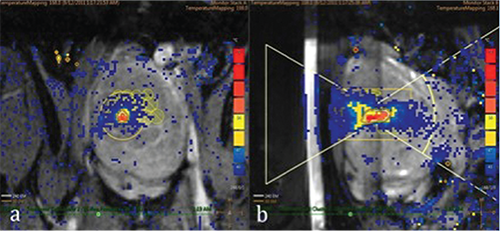
Thanks to soft tissue contrast resolution and thermal mapping capabilities that are superior and more accurate with MR than ultrasound imaging, MRI facilitates treatment planning, visualization of the target, control of energy deposition, and immediate imaging evaluation of treatment response. Current commercial state-of-the-art clinical MRgHIFU systems include ExAblate by Insightec Inc.3 and Sonalleve by Philips,4 deployed on 1.5T or 3.0T MRI platforms. Early clinical applications involve ablation of uterine fibroids, painful bone metastasis, and treatment of essential tremor.5 The first two applications have received FDA approval by InSightec, and various clinical trials are underway for other indications or MRgHIFU systems.
“Uterine fibroids marked the clinical entry point of MRgHIFU applications,” explains Keyvan Farahani (National Cancer Institute). “Unlike traditional oncological therapies, HIFU avoids ionizing radiation and appears to pose no threat of adverse effects from cumulative dose.” The outpatient procedure lasts up to a few hours, depending on the tumor size, and patients typically resume normal activities within a day or two. “For those reasons,” Farahani says, “the scope of potential HIFU applications extend to prostate cancer ablation, liver cancer ablation, vessel occlusion, and disruption of the blood-brain barrier for image-guided drug delivery to the brain for a variety of neurologic and neurooncologic indications.
Before Kullervo Hynynen and Ferenc Jolesz brought HIFU and MRI together, HIFU was severely hamstrung by its inability to offer visual cues on targeting and region of therapeutic effect.
“With MRgHIFU drug delivery, one can deliver thermosensitive carriers, such as liposomes, that can burst at a certain temperature and locally release their therapeutic payload,” Farahani said. Compared to traditional chemotherapy, which takes a more blanket approach, MRgHIFU allows local delivery of high doses of therapy while minimizing systemic uptake. MRI also allows the clinician to immediately view, either directly or with an imaging contrast agent, the extent to which a complicating mass of tissue has been treated.
Now, the technology is branching out to conquer diseases that have confounded medical science for decades, such as Alzheimer’s disease. Earlier this year, Australian scientists6 reported on their study of scanning ultrasound treatments to clear away beta-amyloid plaques in mouse models over six to eight weeks, improving their cognitive function in several domains, including memory and reasoning skills. The research built upon Hynynen’s earlier work, published last year, that showed MRgHIFU treatments to the hippocampus increased neural plasticity and curbed amyloid protein abnormalities.7 And nearly a decade prior, the pioneering duo were locally delivering Herceptin through a disrupted BBB in mice in the pursuit of resolving disorders of the central nervous system.8
Clearly, the technology leaves much to be gained on the back end. “Opportunities for medical physics in HIFU include development of robust quality assurance methods, treatment planning, dosimetry, and treatment monitoring,” explains Farahani, “in addition to training of other scientists and clinicians in proper use of the technology, regulatory, commissioning, and certification roles.”
A recent Research Spotlight article featured MRI as a growing modality in radiation therapy. In fact, there are strong analogies between MRgHIFU and MRgRT as both approaches use external beams of energy and MRI to guide treatments. “The growth of MRgRT will further fuel interest in MRgHIFU as an adjunct or alternative mode of therapy,” Farahani predicts. “There is a long and rich scientific culture associated with radiation therapy that in many ways can provide a model for MRgHIFU, although the requirements for MRgHIFU may be different and at times less demanding since therapeutic effects are readily visualized and measured by MRI.”
To better address the interest of medical physicists in MRgHIFU, AAPM has implemented Task Group 241, whose primary responsibilities include indentifying relevant methodologies, phantoms, and software for performance assessment and clinical applications of MRgHIFU. Technical assessments cover the nuts and bolts of MRgHIFU, the quantitative metrics behind the technology, and pinpointing quality assurance measures and procedures. As with any piece of technology that hopes to disrupt the current landscape, there are economic and competitive challenges that slow progress. To that end, Farahani sees AAPM as a key player for technical assessment, translation to new clinical applications, and development of QA protocols for this emerging technology that has much to offer to the future of medicine and medical physics.
- Cline HE, Schenck JF, Hynynen K, Watkins RD, Souza SP, Jolesz FA. MR-guided focused ultrasound surgery. J Comput Assist Tomogr. 1992 Nov-Dec;16(6):956
- Jolesz FA, Hynynen K, McDannold N, Temapny C. MR imaging-controlled ultrasound ablation: a non-invasive image-guided surgery. Magn Reson Imaging Clin N Am. 2005 Aug; 13(3):45-60.
- www.insightec.com/ExAblate-Operation-Room-Future.html
- www.healthcare.philips.com/main/products/mri/systems/sonalleve/
- Elias WJ, Huss D, Voss T, et. al. A pilot study of focused ultrasound thalamotomy for essential tremor. N Engl J Med. 2013;369(7):640-8.
- Leinenga G, Götz J. Scanning ultrasound removes amyloid-β and restores memory in an Alzheimer’s disease mouse model. Sci. Transl. Med. 2015; 7, 278ra33.
- Burgess A, Dubey S, Yeung S, et al. Alzheimer Disease in a Mouse Model: MR Imaging–guided Focused Ultrasound Targeted to the Hippocampus Opens the Blood-Brain Barrier and Improves Pathologic Abnormalities and Behavior. Radiology. 2014 Dec 273(3).
- Kinoshita M, McDannold N, Jolesz FA, Hynynen K. Noninvasive localized delivery of Herceptin to the mouse brain by MRI-guided focused ultrasound-induced blood-brain barrier disruption. Proc Natl Acad Sci U S A. 2006 Aug 1;103(31):11719-23. Epub 2006 Jul 25.