Virtual Press Room
Press Conference
A PRESS CONFERENCE presenting four important studies from the AAPM Annual Meeting will be held on Tuesday, July 22, 11 a.m. ET (10 a.m. CT), in Room 15, Level 4 of the Austin Convention Center.
The press conference will include research on:

- Radiotherapy for Cardiovascular Disease: New research shows that radiation therapy may offer an alternative treatment for hypertension and atrial fibrillation.
- From Medical Images to Genomics: A study of more than 300 cancer patients utilized information hidden within imaging tests to more accurately identify the radiation dose needed to kill a tumor.
- Data Mining for Improved Cancer Treatment: Medical physicists will present research on their use of data mining of more than 500 head and neck cancer cases to improve outcomes and decrease side effects.
For more information on the press conference, including teleconferencing details for those unable to attend in person, please contact: Ashley Moses at 312-558-1770 or amoses@pcipr.com.
Press Releases
- Innovative Data Collection System For Cancer Patients
Developed To Improve Care, Outcomes
Real-time insights designed to provide personalized approaches for head and neck cancer - Hidden Information Behind Imaging Tests For Cancer May Unlock New Approaches To Radiation Therapy
Emerging field of radiomics can provide insights into cancer treatment success - New Target For Radiation Therapy: Study Suggests Cancer Treatment May Offer Hope Against Heart Disease
For detailed author information, contact: Ashley L. Moses at 312-558-1770 x182 or amoses@pcipr.com.
Hot Topics
The 56th AAPM Annual Meeting features cutting edge research across the field of medical physics science. Six HOT TOPICS from the Scientific Program are summarized below.
The Physics of Cancer
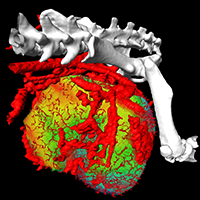 The Science Council Session at this year’s AAPM Annual Meeting focuses on “The Physics of Cancer,” emphasizing fundamental science in understanding how cancer originates, its progression, and its response to treatment. Among the presentations is work by Dr. Robert Jeraj and colleagues at the University of Wisconsin on anti-angiogenic therapy. This emerging form of cancer treatment works by stopping tumors from making new blood vessels, and new research suggests that molecular imaging can be used to help doctors make more informed decisions about its use. Understanding how tumors respond to anti-angiogenic therapies is key to improving a patient’s treatment efficacy. Dr. Jeraj is using molecular imaging, such as FLT PET/CT, to better understand how anti-angiogenic therapies will stop or slow rapid tumor growth.
The Science Council Session at this year’s AAPM Annual Meeting focuses on “The Physics of Cancer,” emphasizing fundamental science in understanding how cancer originates, its progression, and its response to treatment. Among the presentations is work by Dr. Robert Jeraj and colleagues at the University of Wisconsin on anti-angiogenic therapy. This emerging form of cancer treatment works by stopping tumors from making new blood vessels, and new research suggests that molecular imaging can be used to help doctors make more informed decisions about its use. Understanding how tumors respond to anti-angiogenic therapies is key to improving a patient’s treatment efficacy. Dr. Jeraj is using molecular imaging, such as FLT PET/CT, to better understand how anti-angiogenic therapies will stop or slow rapid tumor growth.
Speakers:
R. Jeraj, Ph.D., Associate Professor, University of Wisconsin
D. Low, Ph.D., Professor and Vice Chair of Medical Physics, UCLA
Additional studies related to this topic »
| The Science Council Session | |
| WE-E-17A | The Physics of Cancer Ten oral presentations. Topics include: tumor angiogenesis, predicting cancer treatment response, imaging for cancer prognosis, and mathematical models of cancer biology |
| Scientific Session | |
| MO-G-BRF | The Physics of Cancer (2) Ten oral presentations. Topics include: (TWO Best-in-Physics presentations) PET, CT, MRI, and optical imaging of cancer, computational models of cancer progression and treatment response, and nanotechnology for imaging and therapy. |
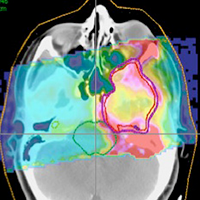
Radiomics: Medical Imaging Meets Genomics in the Fight Against Cancer
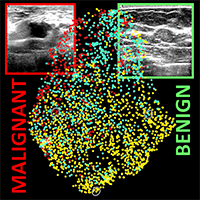 Characteristics of tumors that can remain hidden in medical images are being tested for the ability to predict risk, prognosis and response to cancer therapy. This approach is part of a powerful emerging field in medical physics called radiomics, which seeks to extract statistical information from images to make better treatment decisions. Radiomics research also helps determine how information from medical images can be combined with genomic information from individual patients to improve outcomes. A special session on Monday presents the fundamentals and latest advances in combining quantitative imaging and genomics in the practice of medical physics.
Characteristics of tumors that can remain hidden in medical images are being tested for the ability to predict risk, prognosis and response to cancer therapy. This approach is part of a powerful emerging field in medical physics called radiomics, which seeks to extract statistical information from images to make better treatment decisions. Radiomics research also helps determine how information from medical images can be combined with genomic information from individual patients to improve outcomes. A special session on Monday presents the fundamentals and latest advances in combining quantitative imaging and genomics in the practice of medical physics.
Speakers:
M. Giger, Ph.D., Professor, University of Chicago
M. Cowperthwaite, Ph.D., Medical Informatics Programs Coordinator, Texas Advanced Computing Center, University of Texas
M. Markey, Ph.D., Assistant Professor, University of Texas
Additional studies related to this topic »
| TU-A-12A-7 | CT-Based Biomarkers to Characterize Lung Lesion: Effects of CT Dose, Slice Thickness and Reconstruction Algorithm Based Upon a Phantom Study B Zhao1*, Y Tan1 , W Tsai1 , L Lu1 , L Schwartz1 , Z Lu2 , J So1 , J Goldman1 , (1) Columbia University Medical Center, New York, NY, (2) University of Chicago, Chicago, IL |
| TU-A-12A-10 | Robust Radiomics Feature Quantification Using Semiautomatic Volumetric Segmentation E Rios*, C Parmar , M Jermoumi , H Aerts , Dana-Farber Cancer Institute, Boston, MA |
| WE-E-17A-4 | CT Based Radiomics Data Predicts for Nodal Involvement and Overall Survival in NSCLC T Coroller*, p Grossman , E Rios , R Mak , H Aerts , Dana Farber Cancer Institute / Harvard Medical School, Boston, MA |
| WE-E-17A-3 | FDG-PET-Based Radiomics to Predict Local Control and Survival Following Radiotherapy J Oh*, A Apte , M Folkerts , Z Kohutek , A Wu , A Rimner , N Lee , J Deasy , Memorial Sloan Kettering Cancer Center, New York, NY |
| WE-E-17A-2 | Predictive Modeling of Outcome Following SABR for NSCLC Based On Radiomics of FDG-PET Images R Li*, T Aguilera , D Shultz , D Rubin , M Diehn , B Loo , Stanford University, Stanford, CA |
Patient Safety in Radiotherapy
 Radiation therapy is one of the most complex areas of healthcare and, as such, the delivery of safe, high-quality treatments can be challenging. To address this issue, the AAPM and ASTRO are launching the National Radiation Oncology Incident Learning System, RO-ILS, a platform allowing providers to share information about safety which is critical in this type of environment. An invited symposium on Thursday, July 24, presents the recently launched RO-ILS platform and the implications for improved quality and safety in radiation therapy.
Radiation therapy is one of the most complex areas of healthcare and, as such, the delivery of safe, high-quality treatments can be challenging. To address this issue, the AAPM and ASTRO are launching the National Radiation Oncology Incident Learning System, RO-ILS, a platform allowing providers to share information about safety which is critical in this type of environment. An invited symposium on Thursday, July 24, presents the recently launched RO-ILS platform and the implications for improved quality and safety in radiation therapy.
Speakers:
E. Ford, Ph.D., Associate Professor, University of Washington, Seattle WA
G.Ezzell, Ph.D., Professor and Chief of Physics, Mayo Clinic, Phoenix AZ
B. Miller, MS, Medical Physicist, Henry Ford Health System, Detroit MI
E. Yorke, Ph.D., Attending Physicist, Memorial Sloan-Kettering Cancer Center, New York NY
Additional studies related to this topic »
| SU-E-T-192 | FMEA Severity Scores - Do We Really Know? J Tonigan*, J Johnson, S Kry, P Balter, L Court, F Stingo, D Followill, UT MD Anderson Cancer Center, Houston, TX |
| MO-E-9A-1 | Risk Based Quality Management: TG100 In Action M Huq1*, J Palta2*, P Dunscombe3*, B Thomadsen4*, (1) University of Pittsburgh Medical Center, Pittsburgh, PA, (2) Virginia Commonwealth University, Richmond, VA, (3) Tom Baker Cancer Centre, Calgary, AB, (4) University of Wisconsin, Madison, WI |
| MO-G-BRE-9 | Validating FMEA Against Incident Learning Data: A Study in Stereotactic Body Radiation Therapy F Yang*, N Cao , L Young , J Howard , P Sponseller , W Logan , T Arbuckle , T Korssjoen , J Meyer , E Ford , Department of Radiation Oncology, University of Washington Medical Center, Seattle, WA |
| TU-C-BRE-11 | 3D EPID-Based in Vivo Dosimetry: A Major Step Forward Towards Optimal Quality and Safety in Radiation Oncology Practice B Mijnheer*, A Mans , I Olaciregui-Ruiz , R Rozendaal , H Spreeuw , M van Herk , The Netherlands Cancer Institute, Amsterdam, North Holland |
Advances in CT Imaging, Dose Reduction, and Image Quality
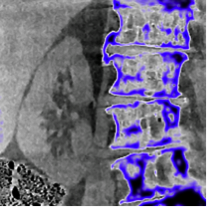 This year marks the 25th anniversary of spiral CT, and ongoing advances in scanner technology, mathematical algorithms, and high-speed computing are converging in a way to advance CT performance while minimizing radiation dose. Advances include: the use of previous CT scans of the same patient to improve quality and reduce subsequent scans; the use of mathematical algorithms to decrease image noise; the use of image-guided surgery to improve surgical guidance and reduce dose; and measuring and modeling image quality to identify dose limits in a manner consistent with the imaging task. In an invited symposium on Monday, July 21, experts from the University of Wisconsin, University of Chicago, Johns Hopkins University, and Duke University present the latest research in these rapidly advancing areas of CT image quality.
This year marks the 25th anniversary of spiral CT, and ongoing advances in scanner technology, mathematical algorithms, and high-speed computing are converging in a way to advance CT performance while minimizing radiation dose. Advances include: the use of previous CT scans of the same patient to improve quality and reduce subsequent scans; the use of mathematical algorithms to decrease image noise; the use of image-guided surgery to improve surgical guidance and reduce dose; and measuring and modeling image quality to identify dose limits in a manner consistent with the imaging task. In an invited symposium on Monday, July 21, experts from the University of Wisconsin, University of Chicago, Johns Hopkins University, and Duke University present the latest research in these rapidly advancing areas of CT image quality.
Speakers:
G. Chen, Ph.D., Professor, University of Wisconsin
X. Pan, Ph.D., Professor, University of Chicago
J. Stayman, Ph.D., Research Assistant Professor, Johns Hopkins University
E. Samei, Ph.D., Professor, Duke University
Additional studies related to this topic »
| SU-F-18C-6 | Prospective Patient Evaluation of Iterative Reconstruction in Radiation Oncology R Price1,2*, S Vance2 , R Cattaneo2 , L Schultz2 , M Elshaikh2 , I Chetty2 , C Glide-Hurst2 , (1) Wayne State University School of Medicine, (2) Henry Ford Health Systems, Detroit, MI |
| MO-PIS-Exhibit Hall-1 | Imaging: CT Dose Optimization Technologies I K Denison1*, S Smith2*, (1) GE Healthcare, Waukesha, WI, (2) Philips Healthcare, Cleveland, OH |
| TU-PIS-Exhibit Hall-1 | CT Dose Optimization Technologies II Driesser1*, E Angel2*, (1) Siemens AG, Forchheim, Germany, (2) Toshiba America Medical Systems, Inc, Tustin, CA |
| WE-G-18A-1 | JUNIOR INVESTIGATOR WINNER - Low-Dose C-Arm Cone-Beam CT with Model-Based Image Reconstruction for High-Quality Guidance of Neurosurgical Intervention A Wang*, J Stayman , Y Otake , G Gallia , J Siewerdsen , Johns Hopkins University, Baltimore, MD |
| TH-A-18C-3 | Noise Correlation in CBCT Projection Data and Its Application for Noise Reduction in Low-Dose CBCT H Zhang1 , L Ouyang2 , J Huang1 , J Ma1 , W Chen1 , J Wang2*, (1) Southern Medical University, Guangzhou, GuangDong, (2) UT Southwestern Medical Center at Dallas, Dallas, Texas |
| TH-C-18A-8 | A Management Tool for CT Dose Monitoring, Analysis, and Protocol Review J Wang1,2*, L Molvin2 , D Marsh2 , C Zorich2 , F Chan1,2 , B Newman1,2 , D Larson1,2 , L Phillips1 , A Leung1,2 , D Fleischmann1,2 , (1) Stanford University, Stanford, CA, (2) Stanford Hospital and Clinics, Stanford, California |
MRI Guidance for Radiation Oncology
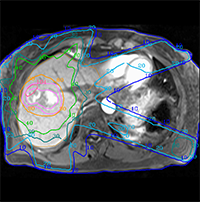 Radiation therapy is benefiting from recent research aimed at integrating MRI into radiotherapy planning and guidance. Recent years have seen the rapid adoption of dedicated MRI systems as simulators that give better visualization of the tumor and surrounding healthy tissue. By bringing MRI directly into the treatment room, new systems offer the potential to guide high-precision radiotherapy by virtue of such improved imaging capability. A special symposium on Tuesday, July 22, features the latest research on bringing MRI into the process of radiotherapy planning, guidance and evaluation of treatment response.
Radiation therapy is benefiting from recent research aimed at integrating MRI into radiotherapy planning and guidance. Recent years have seen the rapid adoption of dedicated MRI systems as simulators that give better visualization of the tumor and surrounding healthy tissue. By bringing MRI directly into the treatment room, new systems offer the potential to guide high-precision radiotherapy by virtue of such improved imaging capability. A special symposium on Tuesday, July 22, features the latest research on bringing MRI into the process of radiotherapy planning, guidance and evaluation of treatment response.
Speakers:
T. Stanescu, Ph.D., Medical Physicist, Princess Margaret Hospital, Toronto ON
J. Balter, Ph.D., Professor, University of Michigan, Ann Arbor MI
T. Nyholm, Ph.D., Senior Lecturer, Umea University, Sweden
J. Lagendijk, Professor, University Medical Centre Utrecht, The Netherlands
Additional studies related to this topic »
| SNAP Oral Session | |
| SU-C-17A | MR-Guided Radiation Therapy Seven oral presentations. Topics include: use of MRI for radiation treatment planning, registration of MRI and CT, and managing patient motion in MRI. |
| Scientific Session | |
| WE-G-17A | MRI in the Treatment Room Nine oral presentations. Topics include: integration of MR scanner and linear accelerator, tumor tracking, physics and engineering of MRI in the treatment room, and MRI guidance of brachytherapy. |
Improving the Effectiveness of Proton Therapy
 A special symposium on Wednesday presents research that is uncovering ways to improve cancer treatment using proton therapy. Proton therapy is already known to be 10 percent more effective than traditional photon radiation therapy by delivering radiation more accurately to the tumor and avoiding healthy tissues. Dr. Harald Paganetti and colleagues at the Massachusetts General Hospital used computer simulations of proton therapy to better understand the reason for treatment failure and side effects by more accurately calculating how protons deposit energy in tissue. Dr. Robert Stewart of the University of Washington will present how biological models can be used to improve understanding of tumor response in proton therapy, and Dr. A. Carabe-Fernandez of the University of Pennsylvania will present new research in biologically-optimized proton therapy.
A special symposium on Wednesday presents research that is uncovering ways to improve cancer treatment using proton therapy. Proton therapy is already known to be 10 percent more effective than traditional photon radiation therapy by delivering radiation more accurately to the tumor and avoiding healthy tissues. Dr. Harald Paganetti and colleagues at the Massachusetts General Hospital used computer simulations of proton therapy to better understand the reason for treatment failure and side effects by more accurately calculating how protons deposit energy in tissue. Dr. Robert Stewart of the University of Washington will present how biological models can be used to improve understanding of tumor response in proton therapy, and Dr. A. Carabe-Fernandez of the University of Pennsylvania will present new research in biologically-optimized proton therapy.
Speakers:
H. Paganetti, Ph.D., Professor, Harvard Medical School, Massachusetts General Hospital, Boston MA
R Stewart, Ph.D., Associate Professor, University of Washington, Seattle WA
A Carabe-Fernandez, Ph.D., Assistant Professor, University of Pennsylvania, Philadelphia PA
Additional studies related to this topic »
| SU-E-T-14 | A Feasibility Study of Using Modified AP Proton Beam for Post-Operative Pancreatic Cancer Therapy X Ding*, A Witztum , O Kenton , F Younan , J Dormer , E Kremmel , H Lin , H Liu , S Tang , S Both , A Kassaee , S Avery , Univ Pennsylvania, Philadelphia, PA |
| WE-D-BRE-3 | Late Toxicity Following Photon Or Proton Radiotherapy in Patients with Brain Tumors R Munbodh, PhD* , X Ding, PhD , L Yin, PhD , S Anamalayil, MSc , J Dorsey, MD,PhD , R Lustig, MD , M Alonso-Basanta, MD,PhD , Department of Radiation Oncology, University of Pennsylvania, Philadelphia, PA |
| WE-E-BRF | INVITED SYMPOSIUM: The ESTRO-AAPM Joint Symposium on Imaging for Proton Treatment Planning and Guidance K. Parodi*, D. Dauvergne*, J. Kruse* |
| WE-E-BRE-7 | High-Throughput Mapping of Proton Biologic Effect L Bronk*, F Guan , M Kerr , J Dinh , U Titt , D Mirkovic , S Lin , R Mohan , D Grosshans , UT MD Anderson Cancer Center, Houston, TX |
| WE-G-BRE-2 | Biological Modeling of Gold Nanoparticle Radiosensitization for Proton Therapy Y Lin*, H Paganetti , J Schuemann , Massachusetts General Hospital & Harvard Medical School, Boston, MA |
| WE-G-BRE-7 | Proton Therapy Enhanced by Tumor-Targeting Gold Nanoparticles: A Pilot in Vivo Experiment at The Proton Therapy Center at MD Anderson Cancer Center T Wolfe*, J Grant , A Wolfe , M Gillin , S Krishnan , MD Anderson Cancer Ctr., Houston, TX |
| TH-A-BRE | INVITED SYMPOSIUM: The Status of Intensity Modulated Proton and Ion Therapy L. Dong*, X. Zhu*, J. Unkelbach*, R. Schulte* |
Featured Interviews
AAPM: The Impact of Imaging in Medical Physics
AAPM President John E. Bayouth, Ph.D., discusses the impact of imaging in medical physics, as well as training that is available through AAPM, with Imaging Technology News Editorial Director Melinda Taschetta-Millane.
Using Radiosurgery for Atrial Fibrillation Cardiac Ablation
Paul Keall, Ph.D., FAAP, professor and NHMRC Australian Fellow at Radiation Physics Laboratory at the University of Sydney, Sydney Medical School, discusses radiosurgery beyond cancer.
Stereotactic Radiotherapy for Renal Sympathetic Nerve Ablation with Peter G. Maxim, Ph.D.
Peter G. Maxim, Ph.D., assistant professor of radiation oncology at Stanford University, discusses stereotactic radiotherapy for renal sympathetic nerve ablation for the treatment of refractory hypertension, and some of the challenges involved, with Imaging Technology News Editorial Director Melinda Taschetta-Millane.
AAPM gratefully acknowledges the cooperation of ITN in conducting this interview and making it available here and on their website - not available.

